adaptive user interfaces in healthcare
Kenny R. Lienhard
Chief Technology Officer
medignition AG
07.02.2021
The healthcare ecosystem has a multitude of stakeholders (e.g., patients, physicians, and nurses) each having specific needs. This makes the design of information technologies in healthcare particular complex. The attempt to fulfill all stakeholder requirements often results in “one size fits all” digital health technologies, which in reality fits no-one. medignition has designed a novel telemedicine technology that dynamically adapts its user interface to the individual user’s specific needs. This article presents our model for building an adaptive telemedicine technology.
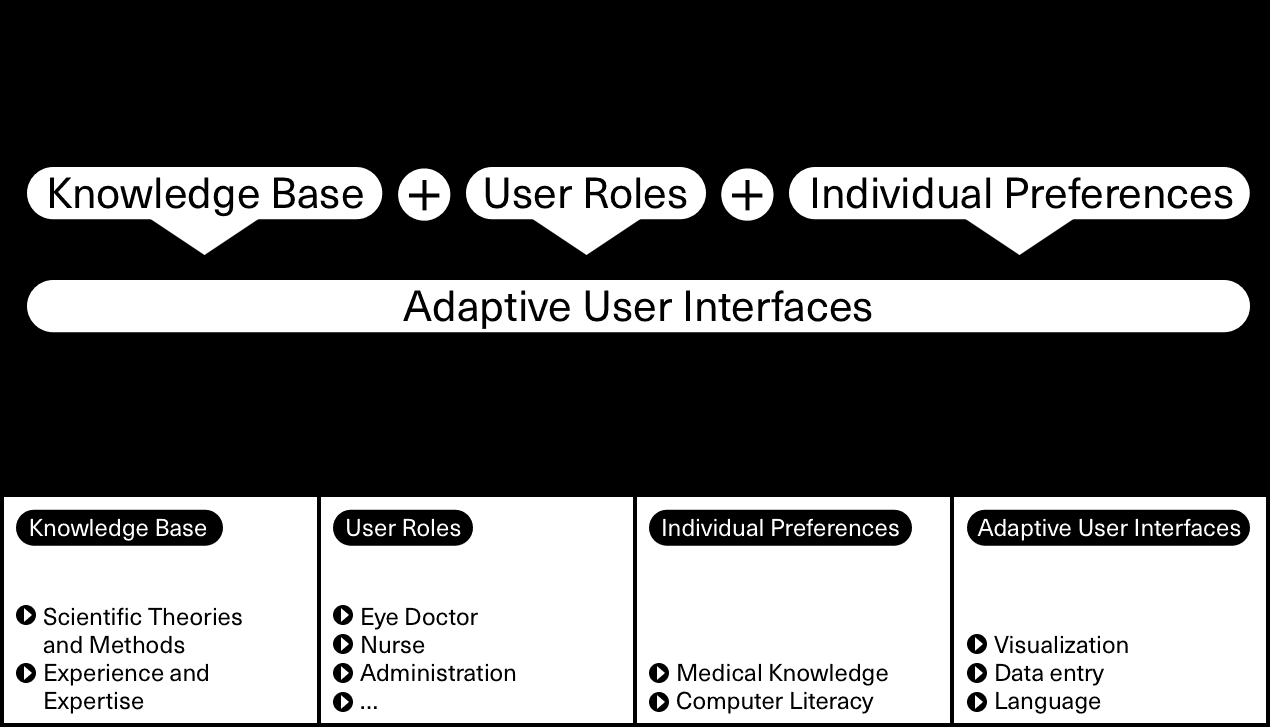
In our research, we have identified three key concepts that guide the individualization of a user interface, namely knowledge base, user roles, and individual preferences. A user interface should use the existing knowledge base (e.g., scientific theories, methods, and experience) as a foundation. Design knowledge informs the way user interfaces look and behave. User interface elements such as primary navigation, search input fields, and data tables reference the knowledge base and make user interfaces more effective, since they are easier to learn, remember, and use. Further, we have defined different user roles that are typically found in a telemedicine service (e.g., nurse, eye doctor, finance, and administration). A user often has multiple roles in service provisioning. For instance, a person might be responsible for both examination planning and invoice tracking. Each role describes a user’s job to fulfill in general, and the required system functionalities and data objects in specific. Individual preferences are the third key concept informing the individualization of a user interface. Past research pointed to medical knowledge and computer literacy as the main drivers for a user’s individual preferences.
Knowledge base, user roles, and individual preferences characterize an adaptive user interface. We have found that adaptive user interface characteristics can be grouped into three elements: language, data entry, and visualization. Language describes, for instance, the way error messages are communicated. Also, the use of jargon might differ between a medical expert (e.g., an eye doctor) and people outside the medical field (e.g., an accountant). Data entry elements may vary since users have different quality management requirements. A patient’s personal contacts, for instance, might be less important for the eye doctor analyzing the patient’s medical data remotely. Valid contact email addresses, however, become crucial when the system informs relatives and associated general practitioners about examination results. Finally, the need for data visualization differs between users that are solely interested in real-time data (e.g., a nurse completing tasks during an examination) and users that aim to see data in context (e.g., an eye doctor looking into the history of medical images).
For our start-up company Augenmobil, we have implemented the model presented here in an innovative telemedicine technology. The model has proven robust in its ability to cope with both initial and future user requirements. Since we have founded Augenmobil in 2019, the telemedicine technology constantly evolved. Our adaptive user interface model provided valuable guidance in this journey.